
Alexis & Joshua
Alexis and Joshua are interested in screening for genetic conditions but want to maximize the chance of getting results with clear next steps

Genetic counseling is the process of helping people understand and adapt to the medical, psychological and familial implications of genetic contributions to disease. This process integrates risk assessment, education and counseling. In some cases, it includes the offer of genetic testing, decision-making support and interpretation of results. Genetic counseling is best provided by specialists with knowledge and experience in clinical genetics, such as board-certified genetic counselors, physician geneticists and advanced-practice nurses trained in genetics.
Genetic counselors, clinical geneticists and nurse specialists in genetics may be available in your institution, or you may need to contact someone elsewhere. If not, you can find genetic specialists through:
Laboratory-based genetic experts can provide information about testing options, benefits, and limitations, as well as help interpreting test results in the context of your patient's history.
It can sometimes be challenging to find a genetic expert locally. In addition to counseling support available through some labs, telecounseling is available through academic institutions and private businesses. In some cases, insurance companies will pay for these remote services. Insurers may be able to provide you a list of covered genetic counseling providers.
Many laboratories offering carrier screening have comprehensive websites that provide educational and practical information about their testing options. Consider the following directories and resources:
Genetic Testing Registry. A resource of the National Center for Biotechnology Information. This registry provides information about clinically available genetic tests and research testing.
Concert Genetics. This company helps users find and compare genetic tests and labs. It can be searched by condition, gene, and test. Labs pay a fee to include information about their tests in the database; clinicians can search the database for free. Concert Genetics can also help clinicians fill out requisition forms online and order testing. Listings include both germline genetic testing for genetic syndromes and genomic testing.
Your own institution's pathology and/or genetics department is often the best first step to finding a lab. Your institution's laboratory may have an established relationship with an outside lab. Check with other labs you use for prenatal testing to see if they offer carrier screening as well.
Some insurance companies have preferred labs for specialty testing, although these may not offer all types of genetic testing. See the section on working with insurance companies below.
Select a reputable, CLIA-certified lab that can work with your institution and the patient's insurance company. In addition, consider the level of guidance you and your patient will need and investigate the support services the lab offers throughout the testing process.
The cost of carrier screening has decreased substantially with advancing technology, allowing higher throughput, but remains variable depending on the laboratory. Carrier screening is generally covered by both public and private insurers in the preconception or pregnancy setting. For uninsured couples, pregnancy may qualify a patient, but not the partner, for coverage under public insurance. For couples with private insurance, screening may be subject to out-of-pocket expenses such as deductibles and co-pays. Some laboratories will provide a cost estimate to patients after insurance verification, and some have programs that assist patients who have limited resources, but it is best to ask the lab directly.
Downstream costs to consider are the cost of partner testing, either concurrent or if the patient screens positive, prenatal diagnostic testing, or preimplantation genetic testing for a specific condition. Insurance coverage may vary for these additional tests. If costs are an issue for a patient, discussions in the future, perhaps before another pregnancy, will provide an opportunity to revisit their options if they are currently unable to participate in screening.
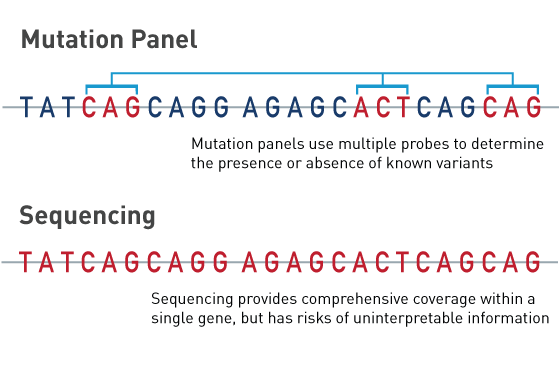
Laboratories currently use two different approaches to carrier screening, mutation panels and sequencing panels.
Mutation panels include individual genetic variants that are associated with disease. These panels can determine the presence or absence of the specific variants, but cannot detect other variants that might be present in the gene. Mutation panels restrict results to common pathogenic variants but have lower sensitivity and detection rates for patients of non-European ancestry.
Sequencing panels detect any changes in the coding portion of the genes (exons). Sequencing assesses all variants in the gene's exons, as opposed to specific variants that have been previously associated with the condition. Using sequencing technology increases the detection rate of less common variants, particularly in underrepresented populations. This approach can detect variants that are known to cause disease, as well as variants that likely cause disease ("likely pathogenic" variants) but cannot be called out as definitively pathogenic. Sequencing may miss gene deletions or duplications.
A laboratory expert can help you understand which technology is utilized by the laboratory and whether reclassification of variants will be reported.
Facilitating informed decision-making in the preconception and prenatal setting can be challenging when testing options are changing rapidly. This is especially true when professional guidelines are not evolving as quickly as technology. Some important topics to incorporate into the informed consent discussion include:
Regardless of which carrier screening option is elected, or if it is declined, the clinicians should discuss other testing and screening options such as aneuploidy screening, chorionic villus sampling (CVS), amniocentesis, newborn screening and cord blood testing.
Carriers of autosomal recessive conditions are not typically expected to have health consequences of a single pathogenic variant. However, as more carriers have been identified, it has become apparent that some recessive genes may have implications for the carrier's health. For example, the recessive neurological condition ataxia telangiectasia is caused by two pathogenic variants in the ATM gene. Carriers of a single ATM variant have a moderately increased risk for certain kinds of cancer. Similarly, Gaucher disease is caused by two pathogenic variants in the GBA gene, while carriers of a single GBA variant have an increased risk of Parkinson’s disease.
Expanded carrier screening panels may also include X-linked conditions, in which a female carrier can have a son with the disease. Female carriers are often unaffected but may exhibit mild features of the disease seen in males or even distinct features unique to carriers. For example, female carriers of Duchenne muscular dystrophy have an increased risk for muscle weakness or cardiomyopathy. Carriers of fragile X syndrome have an increased risk for premature ovarian insufficiency and neurologic disorders such as ataxia. These examples demonstrate the importance of counseling patients on the potential for carrier screening to provide information about their own health status and future risks.
The American Medical Association is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians. The American Medical Association designates this enduring material for a maximum of .5 AMA PRA Category 1 Credit™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
This nursing continuing professional development activity was approved by Northeast Multistate Division, an accredited approver by the American Nurses Credentialing Center's Commission on Accreditation.
In order to claim AMA PRA Category 1 Credit™ or CNE credit, you must: 1) take the preassessment, 2) view the module in its entirety, 3) complete the quiz and evaluation by closing this window and returning to the learning portal where you started the activity.
Already completed this module? If you have already completed this module, you can claim .5 AMA PRA Category 1 Credit™, CNE, or receive a certificate of participation by closing this window and returning to the learning portal where you started this activity.